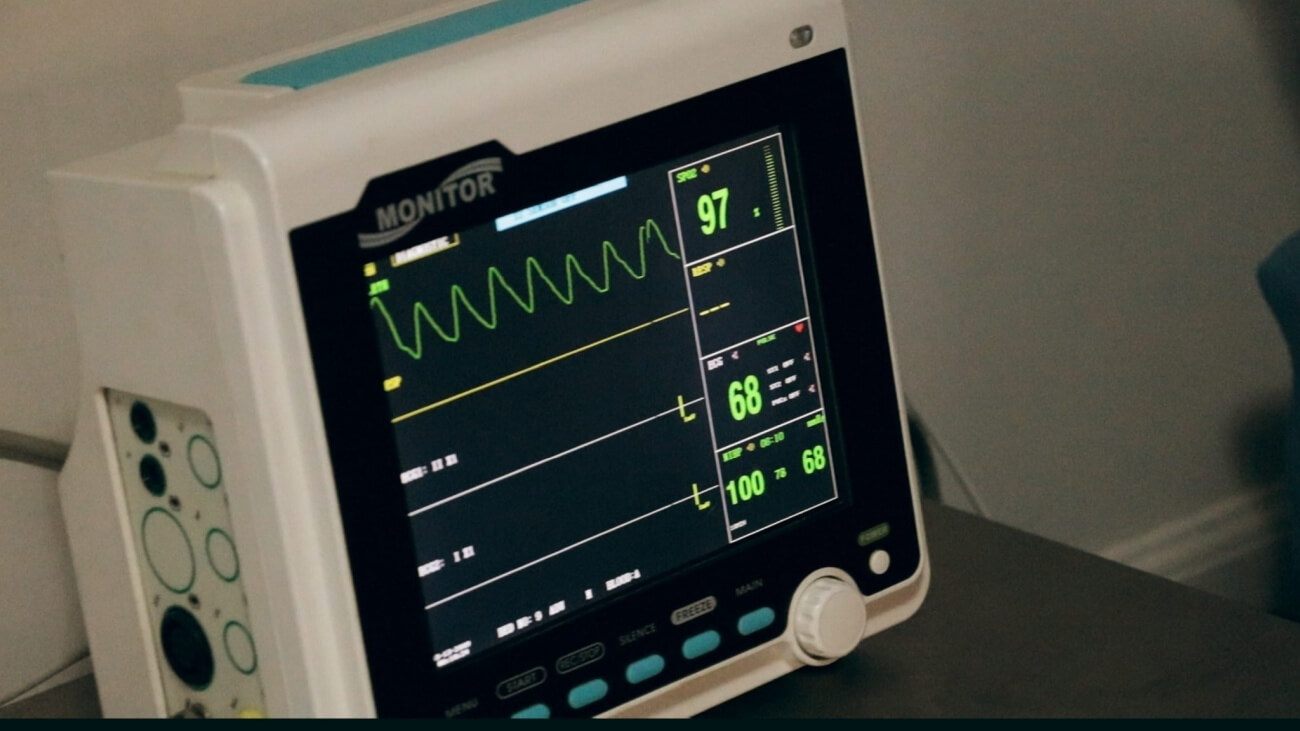
Earlier this year, a report by the National Center for Health Statistics (NCHS) revealed that life expectancy for the non-Hispanic Black population dropped from 74.7 to 72 years between 2019 and the first half of 2020, with the sharpest decline of all groups being for non-Hispanic Black men, whose life expectancy declined by 3.0 years (71.3 to 68.3). The coronavirus pandemic was quickly established as the culprit for this decline, but The Plug spoke to doctors studying this data to understand all the causes behind the decline and what must be done to mitigate or reverse it.
Last year, the world was turned upside down when the Covid-19 virus spread across the world, quickly becoming a pandemic that has killed over 4.5 million people globally. In the United States, the virus has claimed the lives of over 650,000 Americans, but Black Americans incur highest death rates than any other demographic. It is estimated that while 1 in every 1,300 white Americans have died from the virus, that number is 1 in every 380 for Black Americans.
“With the number of deaths that have occurred already in 2021, life expectancy this year will not rebound to pre-pandemic levels,” Theresa Andrasfay, a Postdoctoral Fellow in the Leonard Davis School of Gerontology at the University of Southern California, Los Angeles, told The Plug.
The Associated Press reported that the Centers for Disease Control and Prevention, adjusting for population age differences, estimated that Native Americans, Latinos and Blacks are two to three times more likely than white people to die of Covid-19.
Andrasfay and another researcher looked at reductions in 2020 US life expectancy due to the coronavirus and the disproportionate impact on the Black and Latino populations. Their analysis suggests that the disproportionate impact of the pandemic on Black and Latinos will result in the Black-white life expectancy gap widening while the Latino mortality advantage over whites is expected to narrow.
The leading explanations for why Black and Latinos have disproportionately died from the virus are higher rates of exposure through frontline jobs, greater exposure through crowded living arrangements, having higher rates of comorbid conditions (like obesity and diabetes) and potentially receiving poorer health care, according to Andrasfay and other experts.
“It is extremely important to put this in historical context and not to think of this as an isolated, one-time event in 2020 that affected people of color,” Dr. Steven Woolf, Professor at the Department of Family Medicine and Population Health at Virginia Commonwealth University, told The Plug.
Woolf and his team looked at the effects of the covid-19 pandemic on life expectancy in the US and other high income countries, finding that progress in the last decade to reduce the gap in life expectancy in the US between Black and white people was erased between 2018-20, with life expectancy for Black men dropping to 67.73 years, reaching its lowest level since 1998.
“For generations, it’s been documented, at least from the 19th century forward, that African Americans have experienced higher death rates and lower life expectancy than whites. That is due almost entirely to the legacy of systemic racism,” Woolf said. “There’s no biological reason for it, it has to do with the barriers to the conditions that are important to health, that people of color systematically face as part of their life in America.”
The decrease in life expectancy in the United States was eight and a half times the average of other high-income countries, Dr. Woolf’s study found. The U.S. data was compared to that of Austria, Belgium, Denmark, Finland, France, Israel, Netherlands, New Zealand, Norway, South Korea, Portugal, Spain, Sweden, Switzerland, Taiwan and the United Kingdom.
“One thing it’s important for people to know is that this is not happening in other countries,” Woolf said. “What that tells us is that it didn’t need to be this way. The impact that this pandemic had on Americans was really reflective of the systemic problems we have in the country.”
Social determinants of health refers to the economic and social conditions that influence the quality of life and health outcomes of individuals. These non-physiological factors also affect life expectancy but are often overlooked when implementing policies aimed at improving quality of life and life expectancy.
“Americans tend to think that health is influenced largely by health care. But, and I’m saying this as a doctor, healthcare only accounts for about 10 percent to 20 percent of health outcomes,” Woolf said. “The rest has much to do with our living conditions, what kind of jobs we have, how much income we have, where we live, what resources exist in our neighborhood that promote health, or hazards that endanger our health.”
All of those things have been systematically more adverse to health for communities of color, over the generations,” he said.
“The problem is social determinants have been reduced to poverty, education, income, neighborhood safety, but structural racism, not discrimination, is one of the most most influential social determinants of health in the United States,” Dr. Shervin Assari, Associate Professor of Family Medicine at Charles R Drew University of Medicine and Science, told The Plug.
Dr. Assari has studied the way everyday racism affects Black men in America, finding that racism has been linked to higher levels of death in Black men from suicide, disease and homicide. Dr. Assari has found that, because of racism, associated poverty and injustice, life expectancy at birth for Black men is far below white women, black women and white men.
Dr. Assari’s research has also found that Black men with higher levels of education and higher income are more susceptible to depression and psychological distress, compared to Black women and other demographics.
“This misconception that class protects everyone, income protects everyone, that is a misconception and assumes that there is no race under racism, high income becomes a risk factor for Black men. So if we can fix that thing, that is the biggest step,” Dr. Assari said.