As the United States records its highest number of daily new infections, hospitalizations, and deaths since the pandemic began, with Black Americans contracting the virus and dying at disproportionate rates, one group has committed to ensuring the health and safety of the Black Philadelphia community, risking its own health in the process.
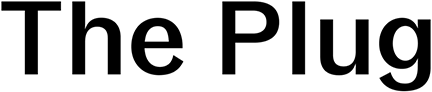
Dr. Ala Stanford, a Philadelphia native and pediatric surgeon at R.E.A.L. Concierge Medicine, a private practice she established, founded the Black Doctors COVID-19 Consortium (BDCC) in mid-April upon learning of the racial disparities in COVID-19 infection rates and deaths, coupled with the lack of testing sites in Black and Brown communities. The Consortium, which also offers free flu shots, was created to provide Southeastern Pennsylvania’s hardest-hit communities with access to barrier-free testing, and has tested over 15,000 people to date, with a positivity rate consistent with the national average. Dates and locations for free testing sites can be found on BDCC’s website, along with the option for people to donate.
“Getting a test was like [looking for a golden ticket in] Willy Wonka and the Chocolate Factory,” said BDCC Chief Operating Officer Kamau Stanford, who is Dr. Stanford’s brother, citing barriers such as insufficient number of symptoms, lack of access to a car, inability to make an appointment, and lack of health insurance. “Essentially, we refused to let people continue to die for access to a $100 test, and refused to let African Americans yet again be relegated to a footnote, or an asterisk in history.”
After first reaching out to the city of Philadelphia to offer her assistance, Dr. Stanford quickly realized there was not a sufficient plan in place for expanding access to testing in Black and Brown communities, and took it upon herself to do so. Recognizing that the most effective way to mitigate contracting and spreading the virus was to enhance testing, Dr. Stanford crowdsourced fellow doctors for tests and personal protective equipment — both of which were hard to come by at the time — before ultimately utilizing her pre-existing relationship with LabCorp to get tests. The largely volunteer-comprised group then rented a van and drove around the neighborhoods, administering tests.
“We had people register on our website if they wanted a test, and we were driving to their houses,” Stanford said. “They would come outside on the corner of their blocks and we would give them their test and then call them back in a couple days with their results. And it just really grew from there.”
The testing initiative was largely self-funded, with the group launching a GoFundMe campaign to raise money for operational costs as well as pay its team. BDCC also took advantage of banks as well as the public sector, through which it was awarded around $1.2 million, Stanford said. Much of the money was distributed by means of a Request for Proposal that was established by the city for any organization that would commit to doing COVID-19 testing in traditionally underserved Philadelphia neighborhoods.
“For every nonprofit that I can think of that exists, the ultimate goal is to work themselves out of a job. If your nonprofit is to help eradicate breast cancer, in a perfect world, there’s a cure for breast cancer, and you’re worked out of a job,” Stanford said. “We really thought we might test for a couple months until the city or state or federal government launched this huge crusade, and then we wouldn’t be needed anymore. In fact, what happened instead was the city realizing and seeing our impact, and funding us.”
The Grim Reality
Black Philadelphians contract COVID-19 at around twice the rate of their white counterparts, as well as are more likely to have severe cases of the virus, according to city data.
Such findings were not surprising for James Garrow, director of communications for the Philadelphia Department of Public Health.
“We saw the racial disparity of the disease really from the very beginning,” Garrow said. “I think everyone was hoping that it wouldn’t be like that, but I don’t think anyone in public health would be surprised to know that a widespread disease like COVID-19 would have outsized effects on folks who have been traditionally underserved and have suffered from so many other epidemics.”
But a study conducted by the University of Pennsylvania’s Perelman School of Medicine suggests that the racial and ethnic gap is wider than what has been reported by health departments in Philadelphia and neighboring suburbs.
According to the study, which tested pregnant women due to their being one of the few populations regardless of race and other factors that continued to frequent the hospital during the height of the pandemic, Black and Latinx women are approximately five times more likely to be exposed to COVID-19 than white women. Scott Hensley, an associate professor of microbiology at the Perelman School of Medicine, said this stark contrast can in part be attributed to systemic racism, adding that the reason the statistic is vastly different from that of the health departments is because results from those departments come from patients who seek testing, while Black and Latinx patients are less likely to get tested due to lack of access to testing and health care in general.

“We need to do studies with larger numbers of individuals to find the underlying reasons why we are seeing these differences in exposures, but it is very likely that these differences are tied to things like differences in socioeconomic status and differences in the ability to socially distance, and all of those things are deep-rooted in systemic racism, and have been going on for many years,” he said, adding that he hopes his findings will lay the groundwork for ensuring equitable distribution of the COVID-19 vaccine.
Many members of the health care field have recently labeled racism its own public health crisis. Stanford agreed, stating that part of the significance of BDCC is that Black doctors test Black patients.
“It’s been well documented in research that Black people have better health care when they are serviced by African Americans, and … cultural competency is the best way to describe it,” he said. “You’re talking to someone who speaks your language, who might be a little bit more empathetic. In a doctor’s office, if you don’t speak a certain way, if you don’t present yourself a certain way, you could easily be dismissed.”
Cheryl Garfield, a community health worker with the University of Pennsylvania Center for Community Health Workers, voiced a similar sentiment, expressing her appreciation for the Consortium after seeing that members of her family were denied testing for not having enough symptoms.
“It lets people in the African American community know that there are people out here that are hearing them, and that those that can, can go somewhere to be tested,” she said.
Looking ahead to 2021
Garrow and Stanford outlined plans to continue their collaboration when delivering the COVID-19 vaccine to the Black Philadelphia community once it is widely available, with Garrow reaffirming the importance of leaning on “the expertise of the folks who know the African American community the best.”
Beyond the vaccine, Garfield stressed the importance of affordable, accessible health care for all.
“Everyone should be treated as humans. It shouldn’t be about what the color of our skin is. It shouldn’t be about where we’re from, or if we’re female or male, or what our education level is, because what does your educational level or your ethnicity have anything to do with the level of care you should receive from a doctor?” she said.
Stanford hopes the Consortium will additionally serve as an educational resource for Black Americans, in which they can learn about individual choices they can make to better their physical health, particularly as COVID-19 continues to target people with pre-existing health conditions such as diabetes.
“What we want to be is an organization that helps educate and provide services in the public health space so that, God forbid, [in the case of another] pandemic, African Americans will not be disproportionately affected still,” he said. “It isn’t about us; it’s about the communities that we serve, the communities that my sister and I are from, and that’s Philadelphia.”
This story is part of a partnership with WURD radio covering technology, business, and innovation in Philadelphia. This vital work is possible with support from the Philadelphia COVID-19 Community Information Fund, an effort by Independence Public Media Foundation (IPMF) and the Knight-Lenfest Local News Transformation Fund (Knight-Lenfest Fund).