Giving birth in the United State can pose a fatal risk. This stark reality became evident to me immediately after I was discharged from a seven-week stay at a public hospital in Ohio, 34 weeks into my pregnancy. There, a team of doctors had monitored my fetus with an uncertain prognosis, constantly warning me of the potential for my daughter to be stillborn and the risk of my own death.
Weeks earlier, I had been labeled by doctors as being a “high-risk” mother: a 30-something African-American with fibroids. Based on the alarming disparity of maternal morbidity and mortality rates between Black and white women in the US, my daughter and I beat the odds. The World Health Organization estimates that about 60,000 expecting mothers in the US suffer birth complications, and close to 1,200 women die every year as a result — numbers that have more than doubled in recent years.
It’s even worse for Black women: Between 2011 to 2014, Black women died at a rate three times higher than white women for every 100,000 live births. Subpar obstetric training and systemic bias are but a few causes for this disparity. A 2017 ProPublica report revealed Black women are more likely to experience risky childbirths regardless of education or class.
New mother and tennis champion Serena Williams has notably become a face for maternal morbidity given her blood clot scare, where her concerns were dismissed. And Black women are less likely to establish a rapport with their doctors, be empowered to make necessary medical decisions or receive empathy from medical staff. A staggering number of these deaths are preventable through better public health strategies, training and access to care.
But the world of tech also may play a role here. There is a growing interest in the use of artificial intelligence in healthcare, including childbirth, that could use algorithms to find better health outcomes for both mothers and their babies. But if the racial and gender bias within the technology is not addressed, it could perpetuate the cycle.
Machine learning, a form of AI, is already used to build self-driving cars and to create facial recognition photo tags on Facebook. In the healthcare industry, artificial intelligence is spoken about in relation to big data, where algorithms are developed based on training datasets to predict risks in patients and manage health outcomes. Philips, PeriGen, and EarlySense are just a few developers of obstetric decision support systems attempting to use of artificial intelligence in perinatal and maternal care.
If the racial and gender bias within the technology is not addressed, it could perpetuate the cycle There are various methods of applying machine learning to obstetrics. Hewlett Packard created a monitoring system using artificial intelligence to predetermine questions physicians can ask high-risk patients based on patients’ recorded medical history.
More modern forms of artificial intelligence use pattern recognition techniques to predict hypertension, preeclampsia and severe maternal morbidity in expectant mothers. One of PeriGen’s AI products, the Early Warning System, continuously monitors vital signs and other health indicators to identify possible threats to the mom or child. EarlySense, meanwhile, monitors a woman’s ovulation cycle and claims to help predict fertility dates.
“One of the promising uses of machine learning in healthcare is the development of algorithms that can process patient data from doctor’s notes to test results and pick up on patterns that may indicate the onset of dangerous conditions that can lead to maternal morbidities, such as infection and sepsis,” Serena Yeung, an incoming professor and researcher at the Stanford Artificial Intelligence Laboratory, told me in an email.
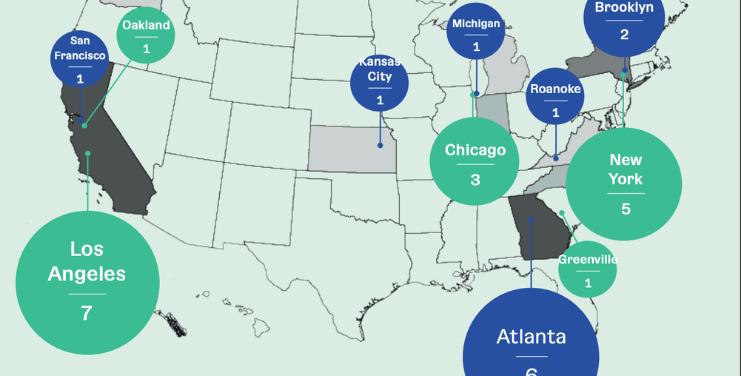
National endeavors have tried to address the morbidity and mortality crisis for Black mothers using data and machine learning. New York City health officials, in conjunction with the De Blasio administration, announced a campaign in July aimed at reducing racial disparities in maternal morbidity. The $12.8 million initiative will include implicit bias training for healthcare providers in addition to the implementation of data tracking techniques to reduce complications in expecting mothers of color.
This story is in partnership with Motherboard. Click here to read the full article.