A new analysis by The New York Times, in partnership with The Marshall Project, found that for every age group Black Americans die prematurely compared to white Americans, particularly that the early death gap is most stark among Black infants. Black babies are more than twice as likely to die as white babies before age one, the analysis found.
The report, which used 2019 data, found that year 3,600 more Black babies died before age one compared to white babies.
The disparities of the health system in the U.S. are rooted in slavery and organizations that uphold and standardize systemic racism. A medical report from 1910 in particular, known as the Flexner Report, had damning and lasting effects on the medical profession in America and helped produce many of the disparities in the number of Black doctors and the continued segregation of patients today.
The report called for reform and the closure of many medical schools across the U.S. and Canada in an effort to make medical studies more segregated and exclusive. The American Medical Associate (AMA), a lobbying group of doctors and medical students which has existed since 1847, took up this same charge that resulted in the profession skewing to mainly include wealthy white male professionals.
The legacy of this system has meant that Black Americans consistently have less and lower quality access to medical treatment than other Americans, according to the New York Times analysis.
But there is a solution—to increase the number of Black doctors.
Research has shown that having more Black doctors leads to better health outcomes for Black patients. For instance, Black infant mortality was halved when the physician caring for the child was also Black. Black men were also more likely to get preventative care when they had Black physicians instead of white.
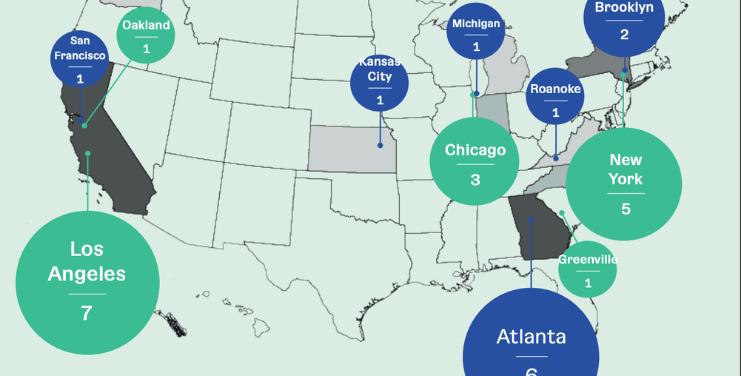
Black doctors are also more likely to use their training to aid underserved communities than white doctors. A 2019 study among medical students conducted by the Association of American Medical Colleges found that 60 percent of Black students planned to practice in underserved communities, compared to 27 percent of white students.
The cost-prohibitive educational requirements to become a doctor has been one barrier to having more Black doctors. In 50 years, the number of Black doctors has only grown by two percent. As of 2019, five percent of doctors in the U.S. were Black.
Medical racism, inequitable and inadequate treatment options and the lack of Black professionals in this field are having a devastating impact on the Black community. Last year, Black male life expectancy dropped by three years, to 68 years old, the largest decline since World War II.
The U.S. is among the only wealthy nations without a universal healthcare system, as such, the medical system functions more like a business in part due to the AMA opposing publicly funded programs. Private industry has stepped up to fill the devastating deadly gaps that exist for Black patients.
It will take a concerted effort to change existing barriers and ensure there is more equity in the next century of medical care.